The Wireless Body
Wireless, wearable health care technologies have long embodied tensions between ideals and markets, transparency and control, and promise and practice.
Nearly half the US adult population will pass out at some point in their lives. Doctors call this “syncope,” and it is bread-and-butter practice for any emergency room or urgent care clinic. While most cases are benign—a symptom of dehydration or mistimed medication—syncope can also be a sign of something gone terribly wrong. It may be a symptom of a heart attack, a blood clot in the lungs, an embolus to the arteries supplying the brain, or a life-threatening arrhythmia. After a series of tests ruling out the worst, most patients go home without incident. Many of them also go home with a Holter monitor.
The Holter monitor is a device about the size of a pack of cards that records the electrical activity of the heart over the course of a day or more. Since its invention more than half a century ago, it has become such a common object in clinical medicine that few pause to consider its origins. But, as the makers of new Wi-Fi and cloud-enabled devices, smartphone apps, and other “wearable” technologies claim to be revolutionizing the world of preventive health care, there is much to learn from the history of this older instrument of medical surveillance.
In 1949, when cardiologist and researcher Norman “Jeff” Holter first imagined a wearable monitor that would broadcast the electrical activity of patients’ hearts as they went about their daily business, he was animated by the newest wireless technology of his day: FM radio. Holter saw radio devices as a way to circumvent the opacity of the body and make physiological processes transparent. In particular, they might reveal hidden disease lurking in the daily fluctuations of the seemingly normal heart. “None of us,” Holter warned a few years later, “knows what transient changes, if any, may occur in the electro-cardiogram of a healthy Cabinet member during the course of an all-day, smoke-filled conference on some international crisis.”
Using Holter’s monitor, the functioning of the ordinary human heart could be continuously tracked, minute by minute. Holter’s ambition wasn’t limited to heart monitors. He envisioned, as he wrote in an article, “a more general project of broadcasting physiological data”—collecting data from people going about their everyday lives and transmitting it to analytic systems for interpretation.
With the right transmitter and the right receiver, wireless technology could access the inner workings of the human body, translate those functions into electronic form, and then broadcast them outside the body. Radio promised health care providers, public health agencies, and employers—along with anyone else who might be interested—the ability to detect disease earlier and to make internal processes legible from the outside. For public health, monitoring society’s hearts en masse offered the grander possibility of preventing heart attacks across the whole population.
As the makers of new Wi-Fi and cloud-enabled devices, smartphone apps, and other “wearable” technologies claim to be revolutionizing the world of preventive health care, there is much to learn from the history of this older instrument of medical surveillance.
The Holter monitor is a reminder that the dream of continuous surveillance of bodily functions through wireless devices did not start in the twenty-first century, or even in the twentieth. Indeed, a repeating cycle of promises and limitations of doing health care better through electronic information technologies can be found well before the digital computer—let alone the internet—became a common feature in clinics and hospitals. This broader history of health care information technology is full of revolutionary promises that never came to pass, and more mundane ones that did.
Dreams (and nightmares) of constant surveillance
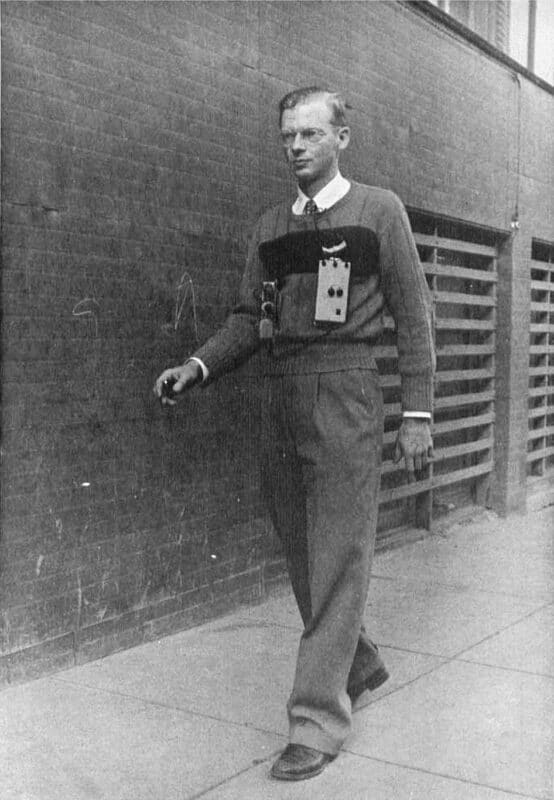
Holter’s first monitor, in 1949, was a bulky FM transmitter hooked up to electrodes on the chest that could broadcast heart tracings a distance of about one city block. When worn by people with known heart lesions, the radioelectrocardiogram could detect abnormalities just as well as a conventional electrocardiogram (ECG) machine, which was developed in 1895. Over the next few years, Holter retooled his device into a smaller form that could fit into a suitcase or satchel. Soon, he believed, anyone would be able to wear one as they went about a normal day.
Holter’s early successes in broadcasting bodily data inspired questions about privacy and how the technology would be applied. In private correspondence, the conservative public opinion researcher Gerald Skibbins joked with Holter that his machine could lead to forms of scientific workplace management that CEOs of the day could only dream of. Firms could monitor the efficiency of blue-collar workers as they performed their daily tasks on the shop floor to “report on any signs of cracking up under the system,” Skibbins speculated. To manage the managers, Skibbins suggested a more exclusive club that would give a member of the executive class “the comfortable frame of mind that his variations from the norm are going to be detected at a time when he can do something about maintaining his efficiency.”
Skibbins was joking—both he and Holter were deeply skeptical of the expansion of the Cold War surveillance state. “I am quite sure,” Skibbins concluded, “that ideas such as these which we take in jest today will be taken seriously by somebody tomorrow.”
Wireless medical devices may have started as the stuff of science fiction, but between the late 1940s and the early 1960s, these technologies laid the foundation for modern physiological tracking. Skibbins’s joke foreshadowed the power that new wearable technologies had, not only in producing new forms of labor management, but in reproducing clear class distinctions (white-collar versus blue-collar, management versus labor) in the design and use of wearable devices. In the fall of 1958, a professor at the Yale School of Forestry reached out to Holter to explore how the device might open new horizons in understanding the physiology of labor in the logging industry, even arranging field trials in forests near Holter’s Montana lab to test the use of the radio-ECG in scientific labor management.
Today, wearable technologies that transmit physiological information in real time are commonplace. Your smartphone or smartwatch can transmit your step count, sleep duration and quality, and pulse rate to a central server for collection and data mining by unknown parties. One out of every five US employers that offered health insurance in 2018 collected wireless physiological information from the wearable devices of their employees. Some firms now use Fitbits, Amazon Halos, and other wearable sensors not just to monitor the health of their workers, but also to optimize their daily work routines. Wireless physiological tracking is simultaneously an opportunity for new health interventions and for newly invasive forms of surveillance. To the casual user, it can be hard to tell for whose benefit tracking apps are designed.
Patients versus markets
Wireless physiological tracking is simultaneously an opportunity for new health interventions and for newly invasive forms of surveillance.
Novel medical technologies regularly arrive wreathed in the language of revolution: every year a parade of new devices promises a paradigm shift that will creatively disrupt or radically transform health care through sudden and absolute change. But the medium of care is never neutral. New communications technologies continuously transform the practice of health care, yet they rarely deliver on promises of increased access to health care for all comers. Nor do they tend to produce the singular acts of disruption celebrated in popular accounts that praise innovators and innovations as the driving force of American medicine, or in the initial public offerings of tech start-ups that monetize their worth. And when electronic communications devices do drive change in medical practice, the changes they bring about often entrench existing power relations just as readily as they overturn them.
When stories are played forward from the past rather than backward from the present, the fate of any given device can be understood as a much more open-ended affair: a speculative repository for broader hopes and fears of designers and users. In the American medical system, where health policy is so deeply entwined with market speculation, the adoption of health communications technologies can carry very different stakes for manufacturers and marketers than it does for practitioners and patients.
The Holter monitor epitomizes this tension between patients and markets. Not long after Holter introduced radiotelemetry as a promising field for clinical practice, a potentially lucrative market for the monitors developed as well. Businessweek and the Wall Street Journal soon projected a growth market for Holter’s devices. With plans in place for a new Electrocardiocorder and Electrocardiocaster, Holter now sought to license these technologies, along with the original Radioelectrocardiograph, to a growing medical electronics industry that could help move his device from a local prototype to a nationally and internationally available consumer good.
Visiting New York to attend the newly established International Conference on Medical Electronics, Holter was encouraged to see that other physiologists and cardiologists were building their own devices for radio-ECGs. Many of these units were still quite heavy: the vacuum-tube equipment developed by one team at the University of Nebraska weighed more than two pounds. But these do-it-yourself physician-inventors, and the manufacturers who joined them for the event, were confident that transistorized circuits would continue to yield smaller and smaller devices. As the size of radiotransmitters continued to shrink, with one “already made small enough for a man to swallow,” the editors of the Journal of the American Medical Association (JAMA) speculated on a medical future in which wireless health tracking devices could literally be consumed. By 1960, teams around the world were working on telemetric pills and sensors that could be inserted inside the patient, like tiny spy satellites.
Thousands of hearts at a time
But this was not the only vision of wireless medicine taking root at midcentury. Another use of surveillance was conceived neither in terms of growth markets for individual patient use nor in the utility of tracking devices for managing labor, but as a technology of public health for screening whole populations at a time. Cesar Caceres, the chief of the new Instrumentation Field Station of the US Public Health Service Division of Chronic Diseases, became a leading figure in the development of biomedical telemetry for public health, where broadcasting the functioning of not one but thousands of hearts at a time was seen as a goal.
When stories are played forward from the past rather than backward from the present, the fate of any given device can be understood as a much more open-ended affair.
A technologist and tinkerer himself, Caceres wanted wireless technology to be ubiquitous, and he was convinced that physicians with some electronics know-how should help build their own new electronic communications devices to serve public health. There was emerging evidence from the field of cardiology suggesting that telemetry could enable simultaneous analysis of data from thousands of patients. A 1964 review in JAMA established the importance of the technology in cardiac intensive care units, which were becoming part of the infrastructure of American hospital care. From that point forward, the continuous remote surveillance of the ailing heart played a key role in reducing the lethality of heart attacks and enabling newer and more effective forms of cardiac surgery.
In theory, radiotelemetry devices could be built by anyone who understood the basics of electronics. So even as Holter began to trademark and license his own devices, which sold for about $1,500, radiotelemetry attracted a cohort of amateur medical technologists. As US Air Force doctor Frederick W. Fasgenelli described in an article titled “Electrocardiography by Do-It-Yourself Radiotelemetry,” DIY approaches to radio-ECG could make the technology available to anyone with $15 for parts and four hours of free time. For radiotelemetry to have its maximal impact, he argued, hospitals should not depend on purchasing expensive devices from medical device and electronics firms, but instead enable their in-house technicians to find affordable means to produce their own.
This open-source model of DIY radiotelemetry spoke directly to Caceres’s hope that accessible wireless medical devices could spawn an entirely new field of public health research into the epidemiology of “silent diseases,” such as diabetes, hypertension, and cancer. Holter’s radioelectrocardiograph didn’t need to be a brand-name product; it could be a generic instrument. Any aspect of bodily function might be made transducible and transmissible for broader study.
The continuous remote surveillance of the ailing heart played a key role in reducing the lethality of heart attacks and enabling newer and more effective forms of cardiac surgery.
Even though the midcentury movement for biomedical telemetry never truly became a DIY project, Caceres succeeded in reimagining physiology as a science of pure information and recasting preventive medicine as a field of big data. With wireless devices, physiological information could be translated into electronic form inside the body, sent across distances ranging from a few feet to hundreds of miles, picked up by a distant receiver, and processed and stored as meaningful information. Guided by the cybernetic theory of Norbert Weiner and the information theory of Claude Shannon, biomedical telemetry became an infinitely modifiable platform for converting more and more functions of the human body into analyzable data. In the hands of public health officials like Caceres, biomedical telemetry promised to transform the study of preventive medicine into a field of transparent and continuous surveillance—especially for the larger time frames and data sets necessary to study the epidemiology of chronic conditions like heart disease.
The expansion of personal health data in public health research also created new problems. As an employee of the US Public Health Service, Caceres favored the adoption of telemetry technologies as part of a benign and expanding surveillance state. Yet he agreed with Skibbins that there was risk as well as potential in the widespread collection of physiological data. Both urged caution. Where would all this data be stored? How would it be protected? What analytic power could make sense of the reams and reams of tracings these new devices collected? As electronic transmissions of physiological processes became transmuted into biomedical data, these challenges of storage and analysis offered a glimpse of the challenges to come. A new crisis of data deluge was on the horizon.
Every patient a radio station
As Holter sought to license and market new radio technologies for collecting bodily data, he wrote that these devices also brought new problems related to “the very voluminous data acquired.” Each Holter monitor could store 24 hours’ worth of ECGs. At an average heart rate of 80 beats per minute, a single device being worn by a single patient for a single day would generate more than 100,000 ECGs to be analyzed. The regular use of just one Holter monitor in any given month could quickly exceed the analytic capacity of an entire small cardiology practice.
Biomedical telemetry promised to transform the study of preventive medicine into a field of transparent and continuous surveillance.
New magnetic storage and digital computing techniques, available by 1960, offered a solution. The first data analysis prototype produced by the Holter Research Foundation, the Audio-Visual Superimposed ECG Presentation, enabled 24 hours of continuous ECG recording to be evaluated in less than 20 minutes. Basically, the doctor played back the recording at 20 times normal speed—both as a visual image on an oscilloscope screen and as an acoustic pattern on a loudspeaker that sounded like a background static “growl.” By scanning the screen and listening to the underlying rhythm, the analyst could revisit any signal of deviation, either seen as a “spike” or heard as a “blip,” by slowing down the playback speed. Accused of adding a depth and volume of data to electrocardiography that cardiologists were simply not yet ready for, Holter countered that “it is in the nature of science sometimes to find oneself working on the roof before the second floor is finished, and this cannot be helped.”
The automation of human telemetry fundamentally changed who had access to this vital medical information. As Caceres had observed, although medical monitoring systems were originally developed by teams of physicians and engineers, in the future their “use will be primarily in the hands of nurses and nonelectrical technicians” who needed simpler interfaces, alerts, and alarms to know when the telemetry of bodily signals indicated danger or required an immediate response. As remote telemetry transformed vital information into electronic data, it also allowed this information to be displayed in real time across visual displays in nurses’ stations equipped with alarms that would sound whenever a parameter deviated. For generations, the ECG had been a cryptic tracing legible to physicians only after years of training. Now, automated alarm systems connected to telemetry monitors allowed more nurses, aides, and technicians to act on previously invisible indicators of a problem. Caceres developed other diagnostic algorithms to automatically detect arrhythmias and signs of heart strain. The effects of the devices were twofold, making the inner functions of the patient’s body more visible to physicians, while also making the art of diagnosis more accessible to nonphysicians.
Although Caceres recognized that radiotelemetry was chiefly used in intensive care units, he was hopeful that monitors might soon be built into the monitoring of every hospital patient. Eventually, every hospital bed could become a relay station in a field of continuous surveillance. “If one thinks of each patient or bed as a radio station and each monitoring apparatus as a receiver,” he explained, “one may observe physiological function by tuning from one ‘station’ to another without any interference.” This vision of ongoing surveillance extended from intensive care unit to the hospital floor, from hospital floor to outpatient clinic, and from outpatient clinic to consumer technologies in everyday homes and workplaces. In turn, as patients became more mobile through smaller and smaller iterations of the Holter monitor, their data were made available to more parties than anyone could have anticipated—whose motivating interests in its collection and analysis might be altogether different from doctor, nurse, or patient.
Technologies we have learned not to see
Whether scanning, smelling, tasting, auscultating, or percussing, physicians had long used their own senses to detect subtle signals of disease. Tools were designed to transcend the limits of those senses. The stethoscope, the thermometer, and the electrocardiogram all represented ways to amplify faint signals from inside the body and make them legible to the outside world. What was new, however, in the Cold War context surrounding the origins of biomedical telemetry was a particular speculative fiction of transparency. Now information could be silently transmitted across the borders of the human body, enabling continuous, remote surveillance of processes within—and arousing anxieties and paranoia. Although many of these fears were associated with broader fears of the surveillance state—both Soviet and American—in hindsight it appears that many of the more insidious uses of wireless surveillance have taken root in the private workplace.
As patients became more mobile through smaller and smaller iterations of the Holter monitor, their data were made available to more parties than anyone could have anticipated.
It might be tempting to read figures like Holter and Caceres as visionaries, but it is far more instructive to read them as figures very much of their time. Holter built pieces of his own present into the device that continues to carry his name today. The infrastructure of electronic patient monitoring and surveillance that took shape in the Cold War moment, and expanded to the monitors, alarms, and alerts common to every hospital floor today, still bears the marks of that earlier era’s concerns with transmission and reception, signal and noise, surveillance and secrecy. Likewise, these beeping and blinking monitors reflect Caceres’s preoccupation with the possibilities of democratizing information and his vision of the benevolent state. But neither man could foresee that the seemingly incidental marketing exclusivities and trade secrets established in the medical device industry in the postwar decades would continue to prioritize innovation over access in the field of medical electronics today.
These problems have not been solved by the passage of time or by the emergence of newer technologies. Increases in data storage capacity and microprocessor speed have made it easier to transmit, store, and analyze physiological information, but they have also compounded problems of a growing data deluge. While new modes of data encryption initially appeared to offer some privacy protections for users of wearable medical devices, recent years have seen a host of concerns about the hacking of wearable medical devices, from pacemakers to insulin pumps. And as Holter’s friend Skibbins predicted, the wireless body is a source of limitless potential interventions to improve individual and public health, but it is also a space of surveillance and control—and loss of control.
In turn, a continuous debate over how electronics will disrupt medicine can be traced back to the mid-twentieth century, if not earlier. These arguments are not abstract. The medium of care is always contested by different parties with very real professional, political, and financial stakes at play. The source of contention has always been an exchange about technology and power. In the name of empowering the health care consumer, technologists present their new platforms as essential passage points for the future of medicine. In the name of defending the humanity of the patient, physicians assert that no technology should displace the doctor from the bedside.
The wireless body is a source of limitless potential interventions to improve individual and public health, but it is also a space of surveillance and control—and loss of control.
At the most fervent moments of speculation, in which the medical promise of new information technologies became most imminent, it seemed impossible that the utopian or dystopian visions they evoked could be so easily forgotten. Yet the most powerful effects of those prior iterations of new information technology that have been absorbed into the American health care system lay in their becoming invisible. As a society, we have simply learned not to see many of these technologies. Not only do we not see the Holter monitor when we look for histories of medical technology, we also do not see the list of prior promises made when these old technologies were new. Promises of equity. Promises of access. Promises of DIY empowerment. Promises of a new form of health care made seamless in a world of pure information. Promises unfulfilled.
Present concerns with the wireless connectedness of the Internet of Things, the allure of artificial intelligence as applied to health care, and other forms of electronic care superficially seem novel, but the history of past wearable technologies has been selectively forgotten. To this day, patient privacy is defined as information given by the patient, rather than information collected by consumer wireless devices. Most of the intimate data which your Fitbit, Halo, Apple Watch, or Android phone collects regarding your physiological status exist outside the protections of the Health Insurance Privacy and Portability Act, which regulates the use and disclosure of patient health information. And the transmission and commodification of contextual bodily data can enable certain state governments now to look inside people in search of crime scenes: by, for example, gaining access to data from phone-based fertility apps to determine whether, when, and where an abortion may have occurred.
The technology itself is neither inherently liberatory nor inherently constraining. Yet as much as wireless monitoring of physiological parameters through wearable technologies has extended the power of preventive medicine, it has also raised profound concerns about the amount of data collected, the privacy of those data, and the ultimate benefits and costs for the increasing number of individuals being screened.
