Pathways to Middle-Skill Allied Health Care Occupations
Better information about the skills required in health occupations and the paths to career advancement could provide opportunities for workers as well as improved health care.
Health care has been a “job engine” for the US economy, given the sector’s historically strong job growth, an aging population, and increasing demand for health care due to the Patient Protection and Affordable Care Act of 2010 (ACA). Health care professions dominate the list of the 20 fastest growing occupations, with growth rates between 25% and 50%, according to data compiled by the federal Bureau of Labor Statistics. With a good demand outlook and the relatively low entry requirements for several of these jobs, health care occupations appear to be a good career path.
Many of the growing health care professions are “middle-skill,” a term with considerable overlap with the term “allied health,” a category that encompasses a diverse and not precisely defined set of careers. The Association of Schools of Allied Health Professions has identified 66 such occupations; the Health Professions Network, a collaborative group representing the leading allied health professions, has identified over 45; and the Commission on Accreditation of Allied Health Education Programs provided accreditation in 2010 to 28 occupations. These jobs may or may not involve direct patient care, and some do not require specialized skill at entry. Many require less than a baccalaureate degree for entry. Table 1 provides a selective list of jobs in health care that do not require a four-year college degree.
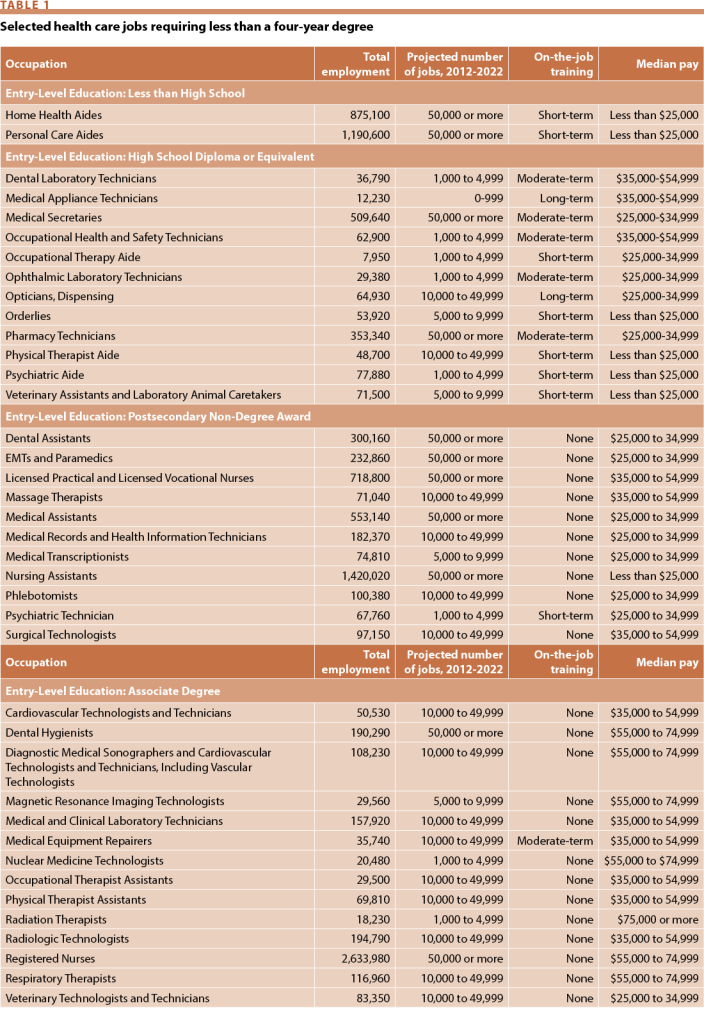
Source: Bureau of Labor Statistics, US Department of Labor, “Occupation Finder,” available at: http://www.bls.gov/ooh/occupation-finder.htm (cited June 12, 2015); Bureau of Labor Statistics, US Department of Labor, “Occupational Employment Statistics, 2012,” available at: http://www.bls.gov/oes/2012/may/oes_nat.htm (cited June 12, 2015).
The pathway to an allied health career can be unclear, especially in relatively new and emerging positions. Clear career pathways and ladders that lead to socioeconomic success need to be clarified in order to direct investments for attracting and retaining a competent workforce. Our task here, then, is to describe what is known about the career pathways into middle-skill allied health careers and the challenges that exist for individuals seeking such careers.
Career pathways and ladders in allied health, as with other health occupations, can be confusing, but making them clearer can help ensure that the nation has a pipeline of skilled workers to deliver high-quality patient care. The first need is to identify potential job areas for people just starting on their career paths. To help identify clear pathways through education into career, the National Association of State Directors of Career Technical Education Consortium developed a National Career Clusters Framework identifying 16 career clusters (including a cluster on health sciences) and 79 career pathways, which the Carl D. Perkins Career and Technical Education Act of 2006 promotes for adoption by educational institutions. The consortium also identified five health science career paths with a common career technical core, knowledge and skill statements, and a plan of study for each of the following pathways: therapeutic services, diagnostic services, health informatics, support services, and biotechnology research and development.
In addition, the National Consortium for Health Science Education developed knowledge-assessment tools and an educational tool clearinghouse for programs in over 300 health science careers. The consortium developed these tools in partnership with six state departments of education, the American Hospital Association, and Kaiser Permanente. By aligning educational tools with the needs of future employers, students will have better preparation for a health care career.
Next comes the need to help those already in the workforce to move up to higher-quality jobs. Several initiatives have been set in motion to help incumbent workers identify career ladders in health care. For instance, the Jobs to Careers Initiative provided incumbent frontline health care workers with on-the-job training as well as career and education planning tools that helped them identify possible career ladders. Another employer-led initiative dedicated to helping low-wage workers identify career ladders is the National Fund for Workforce Solutions. This group has over 20 regional collaboratives and over 30 workforce partnerships focused on the health care sector. They bring together employers, workers, communities, and funders to identify the skills needed by employers and then develop relevant training to help workers gain these skills and advance in their careers. Delivering basic and remedial education, providing strong support and leadership from the employer, and identifying sufficient funding to support training and increase wages are elements that help these programs succeed.
Programs to support a career ladder can improve job satisfaction, reduce turnover, and improve patient care, and they do not necessarily require additional education. The Extended Care Career Ladder Initiative, developed under the Massachusetts Nursing Home Quality Initiative in the early 2000s, represents an early example of an employer-led career ladder program for incumbent health care workers. The initiative brought together nursing homes, home health agencies, community colleges, and regional employment and workforce investment boards to develop career ladders for certified nursing assistants and home health aides. Although the individuals who participated in these programs did not necessarily move into a higher level occupation, the participating organizations saw positive outcomes, such as reduced turnover and vacancies, improved work environments, and improved quality of patient care.
Workers also face challenges in transitioning across occupations. Career transitions across health care occupations are generally rare because pathways are unclear. Although moving among entry-level positions that require no specialized education is relatively simple, moving among highly specialized positions, especially if credentialing is involved, is more difficult—and less likely. A dental hygienist, for example, could potentially move into dental sales but not into nursing without nursing-specific additional education and training. On the other hand, a person with specialized health information technology skills may be able to translate those skills to a non-health care environment.
The career ladder in health care may be better characterized as a career “lattice,” and the myriad education and training choices with different consequences can make career growth and professional development daunting for entrants with minimal education and training or lacking mentors and role models. As students head down one career path, they may realize it is a poor fit and feel uncertain about the next move. Also, some occupations, such as medical assistant, are so new that pathways into other roles, such as a nurse or medical technician, are not yet clear. To make career transitions easier, the US Department of Labor’s Employment and Training Administration is enhancing the Occupational Information Network, or O*NET, which classifies occupations into career clusters in which workers might easily move. O*NET contains information on hundreds of standardized and occupation-specific descriptors. The database, which is available to the public at no cost, is continually updated by surveying a broad range of workers from each occupation. Searching O*NET can help workers identify other jobs that require the same skills.
One motivation for career ladder initiatives is to improve workers’ socioeconomic opportunities. Many allied health care occupations in high demand have low educational entry requirements and are among the lowest paid. A high share of racial and ethnic minorities is in these low-income health care occupations, especially in long-term care settings. Low- and middle-skill workers in long-term care positions generally experience high turnover, high rates of disability, and high rates of poverty. These workers could benefit from opportunities to acquire additional skills and qualify for better-paying positions.
Employers can improve the socioeconomic opportunities for health care workers by supporting on-the-job educational and training opportunities that direct them to career ladders. Having an associate degree and certificates (long-term and short-term) is linked to significantly higher earnings, especially in allied health. Students attending vocational or career technical education programs delivered by community colleges have among the highest rates of returns in earnings relative to other similar educational investments. For those whose education pathways will eventually lead to a bachelor’s degree, starting in community college rather than a four-year college may mean a delay in finishing the higher level degree, but gaining a middle-skill health care occupation could provide financial assistance for meeting higher educational goals.
Supporting education and training
Community and technical colleges are particularly important players in educating the allied health workforce. Private, for-profit institutions are emerging as alternative sources for education and training, although there is some concern about whether they are as cost-effective for students as are the not-for-profit institutions. This is important to policy makers because health care job-specific training opportunities and job assistance programs are often supported through federal and state funds. Public-private partnerships, including apprenticeships, have shown success in training a health care workforce with the skills desired by employers.
In a study of 18 allied health occupations, 62% of the individuals completing a post-secondary program did so at a community college, which may make health care careers more accessible due to a shorter time commitment and lower tuition and living costs compared with four-year programs. Private, for-profit institutions are attracting a growing number of students interested in health care careers. One study by Julie Margetta Morgan and Ellen-Marie Whelan found that 78% of the health care credentials awarded at for-profit institutions were associate degree or non-degree programs for careers that are in high demand. However, many of these students, including a large number of minorities, older students, and otherwise disadvantaged students, experience poor job outcomes, such as high unemployment, lower earnings, and high debt burdens, and they receive a lower rate of return on their educational investment relative to those who received training in non-profit institutions. Education from for-profit institutions may not be perceived well by potential employers. A recent study found that for health jobs that do not require a certificate, applicants with a certificate from a for-profit institution were 57% less likely to receive a callback than applicants with a similar certificate from a public community college.
Federal and state funding programs have attempted to support training programs for students interested in health care careers, with many of the target institutions being community colleges, but the results have been mixed. For example, the American Recovery and Reinvestment Act of 2009 supported 80 community colleges through the Community College Consortia to Educate Information Technology Professionals in Health Care Program. Most of the participants who completed the programs found employment, employers expressed that the hired individuals had the desired competencies, and many of the funded community colleges are continuing their trainings beyond the original two-year grant. However, one-fourth of the community colleges did not continue their programs.
In addition, the Health Profession Opportunity Grants established under the ACA covered educational costs for recipients of support through the Temporary Assistance for Needy Families and other low-income individuals to train into health care jobs that pay well, are in high demand, or both. The most common occupation training course, however, was for “nursing assistant, aide, orderly, or patient care attendant,” which are occupations not well linked to career ladders and upward mobility.
In 2014, the Workforce Innovation and Opportunity Act (WIOA) reauthorized the Workforce Investment Act (WIA) of 1998 with a few key changes. WIA stimulated health workforce development across the states, particularly for occupations requiring short courses of education or training (on-the-job training, certificate programs, and associate degree programs). WIA provided job search assistance, assessment, and training for eligible adults, dislocated workers, and youths under a “work first” mission, and as a result, many allied health occupations were among those pursued by WIA program recipients. WIOA calls for the adoption and expansion of best practices around career pathways, industry or sector partnerships, and the use of industry-recognized certificates and credentials, which opens the opportunity for more rigorous discussions around allied health career pathways. WIOA has been implemented too recently for outcomes to have been assessed.
Employer-provided training and apprenticeships offer another route. Partnerships between employers and educational institutions can ensure that individuals get the competencies their employers need. The Hospital Employee Education and Training program in the state of Washington, a multiemployer training fund that pools resources through collectively bargained employer contributions, supports incumbent hospital workers to attain allied health education prerequisites to become, for example, a clinical lab assistant, emergency department technician, central service technician, or lab assistant/phlebotomist. The Jobs to Career Initiative, supported by the Robert Wood Johnson Foundation, the Hitachi Foundation, and the Department of Labor, brought together 34 employers and served 900 individuals to promote skill and career development in frontline health care workers by integrating curriculum, learning, and assessment into work processes and recruiting co-workers to serve as coaches, mentors, and preceptors.
Apprenticeship programs that provide on-the-job training opportunities are not common in the health care industry, but are being explored. The Department of Labor has identified 10 apprenticeship programs, most of which are allied health occupations, including home health aide, home care aide, pharmacy technician, and medical transcriptionist. Although employers expressed high satisfaction with these apprenticeships as a cost effective way to train and retain workers with desired skills and competencies, they are little-known and often face a lack of resources to ensure oversight of regulated practices.
The accreditation, credentialing, and scope-of-practice measures that help ensure quality care and protect patients from harm can discourage potential allied health workers seeking to follow a career ladder. Credentials required to practice vary by state and by occupation, making it difficult to move from one state to another or follow the career ladder to a new occupation. The cost of credentialing has especially been an issue as job opportunities are expanding across state lines with the increasing use of telehealth services. This barrier not only limits patient access to care, but also the opportunities for allied health workers to grow their skillsets and enter new communities.
Scope-of-practice laws that dictate what a trained worker can and cannot do in an occupation also vary across the country and make interstate moves difficult. Given potential overlaps in skillsets among occupations, competition for job opportunities has caused turf wars over which profession may offer which set of skills in their legal scope of practice. Scope-of-practice laws may hinder team-based environments by limiting practice flexibility that could otherwise enhance delivery of patient care. In areas with workforce shortages, scope-of-practice laws can limit the use of potentially innovative solutions involving shifting tasks from one occupation to another. Recent findings by Kuo et al. and by Spetz et al., published in Health Affairs, suggest that states with less restrictive scope-of-practice laws, specifically for nurse practitioners, result in increased access to care for patients and cost savings.
A path forward
The skills, roles, and education pathways of allied health occupations are changing as health care delivery changes. All health care workers, including middle-skill workers, will need to coordinate and manage care, use technology, work in teams, and help patients navigate the system. The extent to which these new skills and roles are incorporated into current occupations or yield new career categories is not yet clear. For workers to acquire these skills, educational programs and on-the-job trainings must be attuned to this changing health care landscape.
Monitoring the pipeline and supply of allied health professions is a challenge due to the decentralized nature of data collection for allied health professions, especially middle-skill workers, and the highly variable roles that they fill from one employment setting to another, and from state to state. Moreover, since the career pathways to middle-skill allied health occupations are not always clear, capturing data on the educational pipeline of available workers can be a challenge. To track their supply and distribution requires use of data from different sources, each with varying quality, amounts, and types of information.
The available data suggest, however, that pay is relatively low for many entry-level allied health positions and that career ladders may be difficult to identify or are lacking. With increases in reports of high levels of educational debt facing health career students, along with the prominence of for-profit institutions with low returns on employment, individuals should carefully assess their decision to invest in health care careers, especially those requiring low- and middle-level skills.
Given current conditions, then, we offer five recommendations to strengthen the case for entry into middle-skill careers in allied health:
First, research and discussion should be increased to make allied health career pathways more clear, especially for those in the lowest-skilled and potentially low-paying occupations.
Second, interprofessional dialogue should be increased throughout the educational pipeline with health care employers to make sure the right competencies are delivered in a rapidly changing health care landscape.
Third, the apprenticeship opportunities identified by the Department of Labor should be explored as potential avenues for a career path in health care, especially where access to training may be a challenge, such as in rural areas, and for veterans who may have years of experience from the field that could be quickly leveraged into a civilian job.
Fourth, awareness of career opportunities in allied health should be raised by increasing the dissemination of the health science career clusters identified by O*NET and the curricula designed by National Consortium for Health Science Education and National Association of State Directors of Career Technical Education Consortium.
Fifth, a panel of experts should be appointed and charged with regularly monitoring the pulse of the allied health middle-skill workforce, much like the National Health Care Workforce Commission created (but yet to be funded) through the ACA.
These steps comprise a general, though by no means exhaustive, set of actions that may help to improve the prospects for individuals seeking to enter allied health or trying to advance their careers in these fields. They also may help governments and employers build and retain a competent workforce. And they ultimately may lead to improved care for patients in various health settings. Much remains to be done, but the rewards are likely to be commensurate with efforts.
Bianca K. Frogner is an associate professor and health economist in the Department of Family Medicine in the University of Washington’s School of Medicine. Susan M. Skillman is deputy director of the University of Washington Center for Health Workforce Studies.
