Has NIH Lost Its Halo?
After decades of strong budget growth, the National Institutes of Health now faces an increasingly constrained funding environment and questions about the value of its research.
For six decades after World War II, the National Institutes of Health (NIH) was the darling of Congress, a jewel in the crown of the federal government that basked in bipartisan splendor. It enjoyed an open authorization statute, giving it permanent authority to distribute funding without having to come back to Congress to regain that authority every few years. Appropriation hearings to decide the amount NIH would actually spend each year were usually love fests that lasted a week to a fortnight, with each institute and new initiative given its day in the sun. There were tensions and conflict, of course, and members of Congress and disease advocates were persistently disgruntled by NIH’s science-centric culture, perceived to lack urgency to cure cancer or confront the AIDS epidemic. But each year brought concrete accomplishments, examples of how federal dollars had advanced the conquest of disease. It was not just a Potemkin village, but stories of real progress against a common enemy of all humankind, be it cancer, heart disease, stroke, diabetes, Parkinson’s disease, Alzheimer’s disease, or childhood leukemia. The stories were simple and easy to understand, and there was truly a line from NIH research to clinical advances. And plenty of diseases, such as Alzheimer’s, on which all could agree something had to be done, and without research that something would never be clear.
A different disease might catch the congressional eye for a year or three, with boosts for that condition incorporated into a newly elevated budget baseline. Presidents routinely low-balled the NIH’s budget request to make room for their presidential priorities, knowing full well Congress would restore the NIH budget and throw in a bit more.
The result of NIH’s privileged status in Congress was nearly monotonic growth for six decades, punctuated by a few bad years, such as 1967-1969 when two NIH champions left Congress, as Lister Hill retired from the Senate and John Fogarty died, even as James Shannon turned over the reins as NIH director after 13 glorious years of expansion. It took a few years for Mary Lasker and other disease advocates to re-assemble their political coalition, but NIH resumed its expansion into and through the War on Cancer of the early 1970s. Even in the face of considerable controversy over how NIH should be structured and governed, agreement on budget increases was still possible. A few years of relative stagnation in the 1990s gave way to a budget doubling 1998-2003, spanning from the Clinton into the George W. Bush administrations. It mattered little which party controlled the White House or the houses of Congress; everyone is against disease and for research to rid the world of it.
Since that last doubling ended in 2003, however, NIH politics have changed. NIH received one more $10-billion dollop of stimulus funding in 2009-2010 as a swan song for Arlen Specter, honoring his long service, his battle with cancer, and his flip to the Democrats at a crucial moment as he fell off the rapidly eroding moderate edge of the Republican Party. But NIH’s stimulus funding was an anomalous blip in the past decade of budget stagnation. NIH’s purchasing power dropped by double digits after the 2003 peak, and even fear of disease does not seem to overcome the partisan gridlock that besets a Congress likely to be scored the most notoriously dysfunctional in American history. These days, the NIH appropriations hearings are a short and tiny shadow of their former grandeur. The appropriations process itself has largely been replaced by rolling continuing resolutions that extend the previous years’ policies with only incremental adjustments. The days of piling dollars onto NIH are long gone.
This relative neglect of NIH is despite having one of the most politically adept NIH directors in the agency’s history, Francis Collins, who has remarkable capacity for bridging the partisan chasm with folksy charm—buttressed by his guitar and motorcycle—a genuine passion for research and medical care, and talent for explicating biomedical science in human terms.
Are the changing politics a reflection of inattention specific to NIH—a diminution of its perceived importance to Congress or loss of public support—or is NIH merely suffering collateral damage from the larger and deeper paralysis of national government? Is the stagnation simply one among many consequences of polarization and political logjam? Are political undercurrents more permanently changing how federal support for all research will carry into the future? Or do the distinctive features of biomedical politics suggest that its future will be independent of the rest of the federal research and development (R&D) enterprise, as it was during the doubling era? And what might the answers to such questions mean for scientists and decision makers? One place to start is simply by noting that such questions are only now beginning to be asked by the NIH community, and very tentatively at that. The place to start is with an understanding of NIH’s political context, and the fact that the NIH budget rests on several tectonic plates, subject to different political pressures. Here I will explore the dynamics that seem most important for understanding what the future may hold.
Scale escalation
When the NIH budget was $700,000 going into World War II, it was easy to quadruple the budget to $3.4 million by the war’s end, and to boost it another tenfold by the early 1950s. Until the 1970s, the US economy was generally healthy, discretionary budgets floated on rising waters, and NIH got disproportionate increases, both relative to the government as a whole and in comparison to other research agencies (although defense R&D had spurts associated with the Korean War, post-Sputnik, and the War in Vietnam; and the National Aeronautics and Space Administration expanded rapidly in the 1960s to fulfill President Kennedy’s 1961 challenge “of landing a man on the moon and returning him safely to Earth”). From 1970 through 2003, NIH’s research funding consistently and significantly outgrew other federal research accounts (See Figure 1.)
Figure 1
Obligations for basic and applied research, 1970–2009
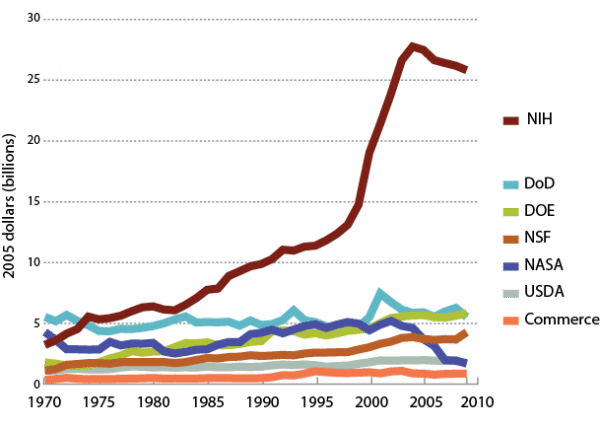
Source: National Science Foundation.
The rise of molecular biology and the continued efforts of disease-research advocates help explain this growth. The promise and practical import of the powerful new molecular and cellular biology were palpable, and Congress fueled their growth through generous NIH budgets. Moreover, NIH was the research arm of a behemoth—the Department of Health and Human Services (or Health, Education and Welfare before President Carter created the Department of Education). NIH began as a relatively small research agency with an ambitious mission in a large department, although after the mid-1960s with the creation of Medicare and Medicaid, most health expenditures through the department were entitlements, not from discretionary appropriations. NIH grew, but so did health expenditures. As a fraction of US health expenditures, the federal health research budget (of which NIH is by far the largest part) has hovered around 2% since 1980.
As NIH’s budget has grown to $30 billion annually—fully half of all civilian R&D expenditures—it has become harder to increase it without pinching other agencies. NIH is now larger than other Public Health Service budgets, so boosting its funding by 10 percent in an era of constrained spending overall would likely cause even larger percent cuts in other vital agencies such as the Food and Drug Administration, Centers for Disease Control and Prevention, Agency for Healthcare Research and Quality, and service components and block grants that are funded by annual appropriations. Appropriations to the Departments of Labor and of Education come out of the same appropriation subcommittee allocation, so NIH also competes directly in the congressional appropriations process with other, non-health programs, including some that are of vital interest to universities (such as the Department of Education’s Pell grants). More broadly, rising entitlement spending puts increasing pressure on all discretionary accounts. Given how well-treated NIH was before the current era of constrained budgets, it is hard to argue that the agency is more deserving of increases than other key agencies.
The annual cures and research breakthroughs, the truly impressive parade of Nobel Prizes and Lasker Awards, and the profusion of research articles that flow from biomedical research excellence tell powerful stories. But the novelty wears off, the frame becomes formulaic, and the hype becomes tiresome, if not defensive. Happy tales do not a healthy dog make. We did not lose the War on Cancer—far from it. Progress has been slow and steady, with some remarkable achievements in drugs for this particular cancer subtype or that. But we have hardly won the war, especially as mortality from metastatic cancer remains largely unabated. After three decades and tens of billions of academic and industrial research dollars poured into the amyloid cascade, there is still no known way to prevent, or even do much to mitigate the ravages of Alzheimer’s disease that threaten to increase inexorably over coming decades. Every year for the better part of a century, members of Congress have heard that cures are “just over the horizon” and that science is poised as it has never been to combat disease. And each year has added to the science base, bringing new scientific opportunities and possibilities for clinical application. Some cures have come, and one after another new technology has opened up new prospects. Knowledge does accumulate. Enthusiasm and novelty, however, do not necessarily follow. New technologies have helped feed rising costs, and the chronic conditions of an aging population grow more intractable. The stories of progress can all be true, but the arguments for larger budgets and more political determination lose their oomph after decades of annual repetition and continued health challenges.
Fractured constituencies
Mary Lasker and Florence Mahoney discovered a political strategy for using private philanthropic capital to leverage biomedical research funding from Congress in the years after World War II. Lasker remained a major figure in the biomedical research lobby until her death in 1994. The AIDS community, meanwhile, had shown how patient groups could be extremely effective at garnering research support, but the political process was becoming more complex. Hundreds of disease groups were by then following the same script that Lasker used to boost cancer research, lobbying to create institutes for their own conditions. And NIH institutes proliferated to respond to these constituencies. Some were for stages of life (childhood and aging), some were for health research fields that were said to be neglected (nursing and biomedical engineering), some were for medical conditions (arthritis, eye disease, communication disorders), and some were responses to scientific opportunity (the Human Genome Project). The biomedical lobby became more factious, more specialized, and harder to harness into a coherent movement for biomedical research as a whole. What was once a War on Cancer became coalitions for particular forms of cancer (leukemia and lymphoma, breast cancer, prostate cancer, “neglected” cancers), and even those coalitions have become fractionated. Breast cancer alone has previvors (those at genetic risk), survivors, and metavivors (those contending with metastatic disease). The subgroups all argue for increased research, but their priorities are not fully in alignment, and some have grown frustrated with NIH’s focus on research rather than cures. The day when just a few activists dominated the political scene has given way to coalitions and sometimes cacophony among research advocates. The number of organizations and their disparate goals diffuse political focus. The politics are more factious, with many constituencies finding their own congressional champions and channels of communication and even, as with the Congressionally Directed Medical Research Programs at Department of Defense, alternative agencies.
As NIH grew, so did the institutions it funded to do research. NIH-funded research, is an industry that sustains academic health centers throughout the nation—and fuels ambitions among every research university to attract a bigger piece of the pie. That industry sometimes behaves as political scientists predict, as an interest group, building national organizations and crafting political strategies to influence elected and executive branch officials in Washington. Academic health centers have expanded remarkably over the decades, and entire careers are devoted to biomedical research lobbying. With such institutionalization comes sclerosis, especially as the system was built on the assumption of infinite growth, and includes no options for responding to resource constraints.
Thus, as Bruce Alberts, Shirley Tilghman, Harold Varmus and Mark Kirchner noted recently in Proceedings of the National Academy of Sciences, biomedical research institutions have trained graduate students and postdocs for research careers that can only accommodate a sixth of their number. Hyper-competition and plummeting success rates are a result of a mismatch between research labor supply and demand. Although exacerbated by stagnant funding, these stresses were inevitable consequences of the system’s growth-dependent dynamics.
As Geoff Earle reported in The Hill, when NIH’s budget was up for discussion soon after its doubling, in March 2004, Senator Pete Domenici, a long-time supporter of NIH and passionate advocate for mental health, exclaimed in frustration:
- “I hate to say it, but the NIH is one of the best agencies in the world,” an angry Domenici said as he spoke in opposition to an amendment by Sen. Arlen Specter (R-Pa.) to boost NIH funding by $1.5 billion. “But they’ve turned into pigs. You know, pigs! They can’t keep their oinks closed. They send a Senator down there [to] argue as if they’re broke.”
After decades of disproportionate growth of the biomedical research sector, the debate after 2003 turned to restoring some balance among funding streams to the physical sciences, engineering, mathematics, and the social and behavioral sciences.
Despite its name, NIH’s mission has not generally been current health per se, but rather research for tomorrow’s health, and progress against intractable diseases through better understanding. An agency devoted to current health would do well to focus on tobacco control, exercise, nutrition, sanitation, and more cost-effective delivery of health care—prevention and efficiency, rather than research on diseases currently not treatable. NIH does these things—some programs such as the National High Blood Pressure Education Program and the National Cancer Institute’s ASSIST program have been signal successes in achieving health gains—but health and health care are not NIH’s main show. NIH is primarily about addressing diseases currently refractory to treatment, in hopes of changing that fact. And that is surely an appropriate government mission, since it is inherently long-term, the main output is information and knowledge, and the financial benefits are hard for private firms to appropriate. These are all features of public goods that only collective action and patient, public capital can supply.
It is a completely fair and open question, however, how much research should focus on basic biological mechanisms, how much on clinically promising interventions, how much on understanding and improving the way health care and preventive services are delivered, and how much on patient-centered outcomes research. It is also fair to ask whether the different elements of the biomedical innovation ecosystem are working well together—and if they are not, what good it would do to continue to favor the biological research approaches. Such questions are especially pertinent in light of the nation’s continually mediocre public health outcomes, and their stark contrast to the sophistication and productivity of the biomedical research enterprise.
One report after another, dating back to the Shannon Era in the 1950s, has tried to address how to achieve the right balance in the research portfolio. The truth is that there is no overarching theory of biomedical innovation sufficient to specify a “right” balance with any precision. At the macro level, Congress appropriates to institutes and centers that map to diseases, health missions, or health constituencies—factors that weigh in the political assessment of social value. At the micro level, most project funding decisions are made by merit review—usually peer review—as a fair way to assess scientific opportunity. The contending factions arguing before Congress help set the macro goals, expert scientists (sometimes augmented by disease-research advocates) make the project-by-project funding decisions, and overall system priorities and institutional architectures evolve to reconcile these different scales. This is a political process solution to a wicked problem with no reliable predictive theory. It is probably not optimal; but the question of what would work better has no agreed-upon answer.
Everyone is against cancer, but not everyone favors human embryo research, or all forms of it. Although the advance of biomedical research is a nearly universal goal, a significant fraction of the polity does not believe in Darwinian evolution, and yet almost everyone who does biology or practices medicine does. This clash of epistemologies carries political risk. As American politics has polarized, some aspects of biomedical research have broken along roughly partisan lines. Stem cell research sharply distinguished the Republican and Democrat platforms in the 2000 and 2004 presidential campaigns, for example, although the partisan differences amplified sometimes relatively small differences in the parties’ actual policy preferences. Embryonic cell research was an unusual intrusion of a biomedical research issue into presidential politics, but it exemplifies the risk. Partisanship over stem cell research did not spill over to affect the overall biomedical research budget, although it did affect the degree to which different administrations set constraints on embryo and stem cell research within the biomedical research budget.
The intensity of partisan discord was less prominent in the 2008 and 2012 presidential election cycles, and only time can tell if biomedical research becomes entangled in partisan bickering. If the intensity of partisanship further escalates, a partisan cleavage could emerge again, and it could affect support for biomedical research in general, not just specific research approaches.
Time for rethinking
Michael Crow, president of Arizona State University, wrote in Nature three years ago about how health research was unduly decoupled from health outcomes, and called for re-thinking how NIH and other components of biomedical research might more directly contribute to better health. I and others responded with concern. We were worried because in a blizzard, it is generally not good policy to shoot the lead dog. NIH is an effective agency, and it was no small feat to establish and sustain its excellence. But the “rethinking” part of Crow’s exhortation is well taken, and there are very large imbalances in the health research portfolio, with health services research and prevention the perennial stepchildren, and biomedical research the favored biological child.
If we turn explicit attention to fostering economic growth and to a focus on more tightly connecting research to its intended goal of improving health, then there is the possibility of not simply growing the crusty, large, and inertial system of health research but also more fully integrating it into the national economy as a matter of national policy.
The prospect is exciting but daunting. Current policies of regulating and paying for health goods and services reward introduction and overuse of expensive technologies that add incremental improvements in health, but with scant attention to cost or relative effectiveness. The trillion-dollar annual federal expenditures through Medicare, Medicaid, and other health programs (such as the Veterans Administration, military health programs, Indian Health Service, and federal employee health program) are not guided by a long-term strategy for improving health care. Instead, they have become open-ended entitlements with brainless purchasing policies. The Medicare statute, for example, explicitly denies authority to consider cost-effectiveness in medical practice, which sets up perverse incentives for cost-escalating innovation. Federal programs are not prudent buyers of the most effective health goods and services. The incentives favor expensive new drugs and devices that command high profit, and discourage low-cost innovation. To call this a “system” or a “market” is to stretch those words beyond coherence.
One obvious response to incoherence is better theory and more facts. It is, however, ultimately unsatisfying to merely call for more research on research. Some gaps are obvious: we need public funding to compare effectiveness of medical goods and services. Private firms’ interests will not drive the knowledge needed to make prudent purchasing decisions. Such information is a public good and the public will have to pay for it. The current laissez-faire approach merely invites perpetual cost escalation. More explicit attention to understanding the current “market” incentives, and to thinking through how to align such incentives for innovation with long-term cost-effectiveness, could contribute to a system that incrementally improves over time, based on evidence. And of course we need more research, both basic and clinical, on diseases we do not know how to control in hopes that someday we will be able to do something about them. In the end, however, how much to spend on research is a political choice, and it will be decided through our political processes.
The decade of stagnation in biomedical research may itself be turning into a political issue. Representatives Fred Upton (R-Michigan) and Diana DeGette (D-Colorado) of the Energy and Commerce Committee (which authorizes NIH activities in the House) are co-leading a bipartisan focus on “21st Century Cures.” This initiative seems to be a traditional bipartisan response, and carries on the congressional legacy of focusing on the conquest of disease. Both features are welcome, but the question is whether they can thrive in the generally poisonous atmosphere in the Capitol.
The importance of research as a component of economic growth is another shared value that can command bipartisan consensus. Elizabeth Popp Berman clearly traces how Creating the Market University grafted a new mission onto the traditional academic goals of creating and disseminating knowledge. Although research universities have had strong and productive ties with industry since the late 19th century, only more recently have they explicitly taken on the mantle of fostering economic growth as key components in a national system of innovation. This analytical framework ripened into national policies, particularly between 1980 and 2000. Recent reports such as Restoring the Foundation from the American Academy of Arts and Sciences, and the National Research Council’s Rising Above the Gathering Storm and its sequels build on this theme.
The kernel of truth in such reports is that universities and research clearly are important sources of ideas, information, and technologies that matter immensely in the innovation ecosystem. One difficulty with the framework, however, is that it relies on open-ended arguments that support increased funding but offer less guidance about how to make investments in economic growth more effective. No coherent theories predict how best to spend public dollars—or tell us how many dollars are enough. The reports are persuasive in documenting stagnation, and about the danger of under-investment and trends pointing to the emergence of R&D-driven economic policies in Asia that could overtake US pre-eminence in research and knowledge-based economic growth. They are, however, also unconvincing in articulating research-system designs that can meet the challenges of today’s world.
The open question for NIH is whether these arguments about economic growth, when combined with the attractive logic of boosting support for research to address the burden of diseases for which current public health and medical care are inadequate, will build political momentum to reverse a decade of neglect. Has NIH lost its halo, or will it begin to shine again?
Robert Cook-Deegan (bob.cd@duke.edu) is a research professor at the Sanford School of Public Policy, Duke University.
